Does the HPV Vaccine Prevent Cervical Cancer?
January 12, 2026
10 minute read
You’re researching HPV vaccination because you want to know if it works. The NHS recommends the vaccine for cervical cancer prevention, but you’ve seen conflicting information online and want to see the actual evidence. Maybe you’re in your 30s wondering if vaccination at your age makes any difference. Or perhaps you’re a parent trying to decide about your teenager’s vaccination.
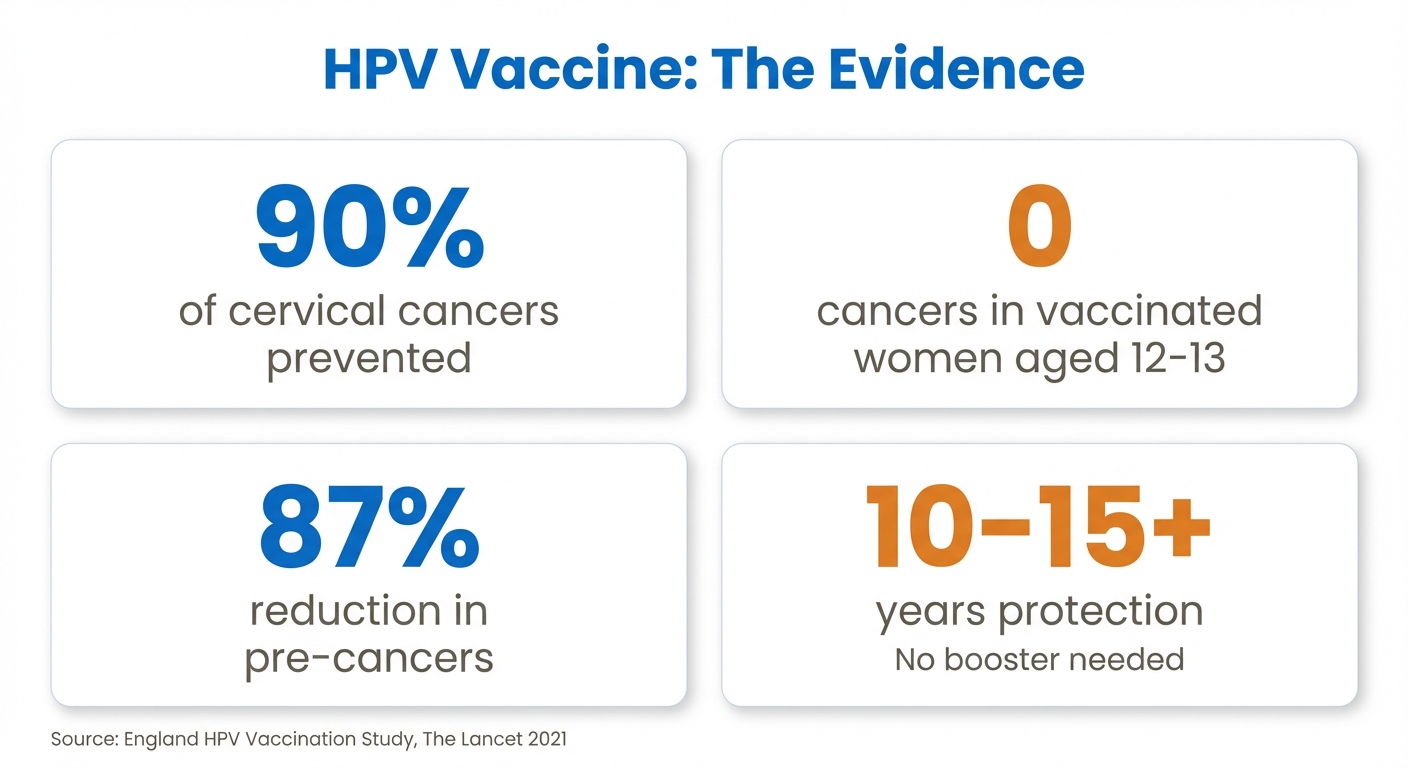
The short answer: Yes, the HPV vaccine prevents 90% of cervical cancers. Studies from England show zero cervical cancers in women fully vaccinated at ages 12-13. But you deserve more than a simple yes – you need to see the evidence.
At Ealing Travel Clinic in West London, we provide Gardasil 9 vaccination for £150 per dose with full transparency about what it prevents and how effective it is. Whether you’re catching up on missed doses or protecting yourself as an adult, the evidence for cervical cancer prevention is stronger than for almost any other vaccine. Most people need 2 doses (£300 total) given 6 months apart. Call us on 0208 567 0982 or visit us at 30 Northfield Avenue, London W13 9RL.
For more detailed information about HPV types and vaccination, see our complete guide to HPV vaccine in London.
The Evidence: How Well Does HPV Vaccine Prevent Cervical Cancer?
The data from real-world vaccination programmes is remarkable. When countries started vaccinating against HPV, cervical cancer rates plummeted.
UK Results (2008-2019 Vaccination Programme)
A major study published in The Lancet tracked millions of women vaccinated in England’s HPV programme:
- Zero cervical cancers diagnosed in women fully vaccinated at ages 12-13
- 87% reduction in cervical pre-cancers (CIN3) in vaccinated groups
- 97% reduction in CIN3 caused by HPV types 16/18 (the main cancer-causing types)
- 34% reduction in cervical cancer rates overall since vaccination started
The study compared outcomes for:
- Women vaccinated at 12-13: Zero cervical cancers
- Women vaccinated at 14-16: 62% reduction in cervical cancer
- Women vaccinated at 16-18: 34% reduction in cervical cancer
- Unvaccinated women: Baseline cancer rates
Earlier vaccination gives better protection, but even vaccination in late teens significantly reduces cervical cancer risk.
Scotland’s Data (2008-2021)
Scotland’s vaccination programme showed:
- 89% reduction in pre-cancerous cervical disease in vaccinated women
- Rates approaching zero for HPV 16/18 infections in vaccinated groups
- Herd immunity effects protecting unvaccinated individuals
Global Evidence
Studies from Australia, Denmark, Sweden, and the United States confirm:
- 90-99% reduction in HPV 16/18 infections in vaccinated populations
- Dramatic falls in genital warts (often the first visible sign of vaccine effectiveness)
- Declining rates of all HPV-related cancers in vaccinated age groups

Zero Cervical Cancers in Vaccinated Women
The England study tracking over 28,000 cervical cancers found zero cases in women fully vaccinated at 12-13 years old. This isn't "might prevent" or "probably helps" – this is elimination of cervical cancer in properly vaccinated women. For comparison, even excellent vaccines like MMR show some breakthrough cases. The HPV vaccine's performance exceeds expectations.
For more detailed information about HPV types and vaccination, see our complete guide to HPV vaccine in London.
How Does HPV Vaccine Prevent Cervical Cancer?
The vaccine works by interrupting cancer development at the very first step.
The HPV-Cancer Connection
HPV doesn’t directly cause cancer. The process works like this:
- HPV infection occurs through skin-to-skin contact during sexual activity
- Persistent infection develops when immune system fails to clear the virus (10-20% of infections)
- Cell changes begin in the cervix (CIN1, progressing to CIN2, then CIN3)
- Pre-cancer develops (cervical intraepithelial neoplasia grade 3)
- Invasive cancer appears years or decades later (if untreated)
This process typically takes 10-20 years. The vaccine interrupts it at the very first step.
Ready to get vaccinated? HPV vaccination in London at Ealing Travel Clinic costs £150 per dose with same-day appointments available. Read more here.
Vaccine Protection Mechanism
Gardasil 9 contains virus-like particles (VLPs) that look like HPV to your immune system but contain no viral DNA. When you receive the vaccine:
- Immune response triggers immediately after first dose
- Antibodies develop specifically targeting nine HPV types
- Memory cells form providing long-lasting protection
- High antibody levels persist for at least 10 years (probably lifetime)
When you encounter real HPV after vaccination:
- Antibodies recognise the virus immediately
- Immune response activates before infection establishes
- Virus cleared before it can cause persistent infection
- No cell changes occur because infection prevented
It’s prevention at the earliest possible stage – stopping infection before it starts.

Which HPV Types Cause Cervical Cancer?
Gardasil 9 protects against the nine HPV types that matter most:
Cancer-causing types:
- HPV 16: Causes 55-60% of cervical cancers
- HPV 18: Causes 15-20% of cervical cancers
- HPV 31, 33, 45, 52, 58: Together cause another 15-20% of cervical cancers
Total cervical cancer prevention: 90% of cases
Wart-causing types:
- HPV 6 and 11: Cause 90% of genital warts
The vaccine doesn’t protect against every HPV type (there are over 200), but it covers the nine types responsible for 90% of cervical cancers. That’s why cervical screening remains important even after vaccination – to catch the remaining 10%.
Does HPV Vaccine Work If You’re Already Sexually Active?
A common misconception about HPV vaccination is that it only works for virgins. This is false.
Protection After Sexual Activity Begins
Clinical trials and real-world studies show significant protection even when vaccinated after sexual activity begins.
This works because:
Most people don’t encounter all nine vaccine-covered HPV types before vaccination. Even if you’ve had one HPV infection, you probably haven’t had all nine types. The vaccine still protects against the types you haven’t encountered.
Studies show:
- Ages 25-45: Significant reduction in new HPV infections post-vaccination
- Women with previous HPV: Still benefit from protection against other types
- After treatment for CIN: Vaccination may reduce recurrence risk
Age and Effectiveness
The vaccine effectiveness by age:
- Ages 9-14: 96-100% effectiveness (pre-sexual activity)
- Ages 15-26: 70-90% effectiveness (some may have encountered HPV types)
- Ages 27-45: 50-70% effectiveness at population level (likely encountered some types, but still protects against others)
The vaccine itself works just as well at any age. Lower effectiveness at population level reflects that some adults have already encountered certain HPV types. But you’re still fully protected against types you haven’t had.
Real-World Example
A 30-year-old woman gets vaccinated:
- She might have had HPV 16 in the past (cleared by her immune system)
- She’s probably never had HPV 31, 33, 45, 52, or 58
- The vaccine provides full protection against these types
- She’s now protected against 60-70% of cervical cancers she wasn’t previously protected against
That’s still enormous benefit.
Protection Even After HPV Exposure
Even if you've been sexually active for years, HPV vaccination provides significant cervical cancer prevention. You're unlikely to have encountered all nine vaccine types. Studies of adults aged 27-45 found vaccination provided significant protection against vaccine-covered HPV types they hadn't yet encountered, preventing the majority of related cervical disease. It's never too late for protection.
Ready to get vaccinated? HPV vaccination in London at Ealing Travel Clinic costs £150 per dose with same-day appointments available.
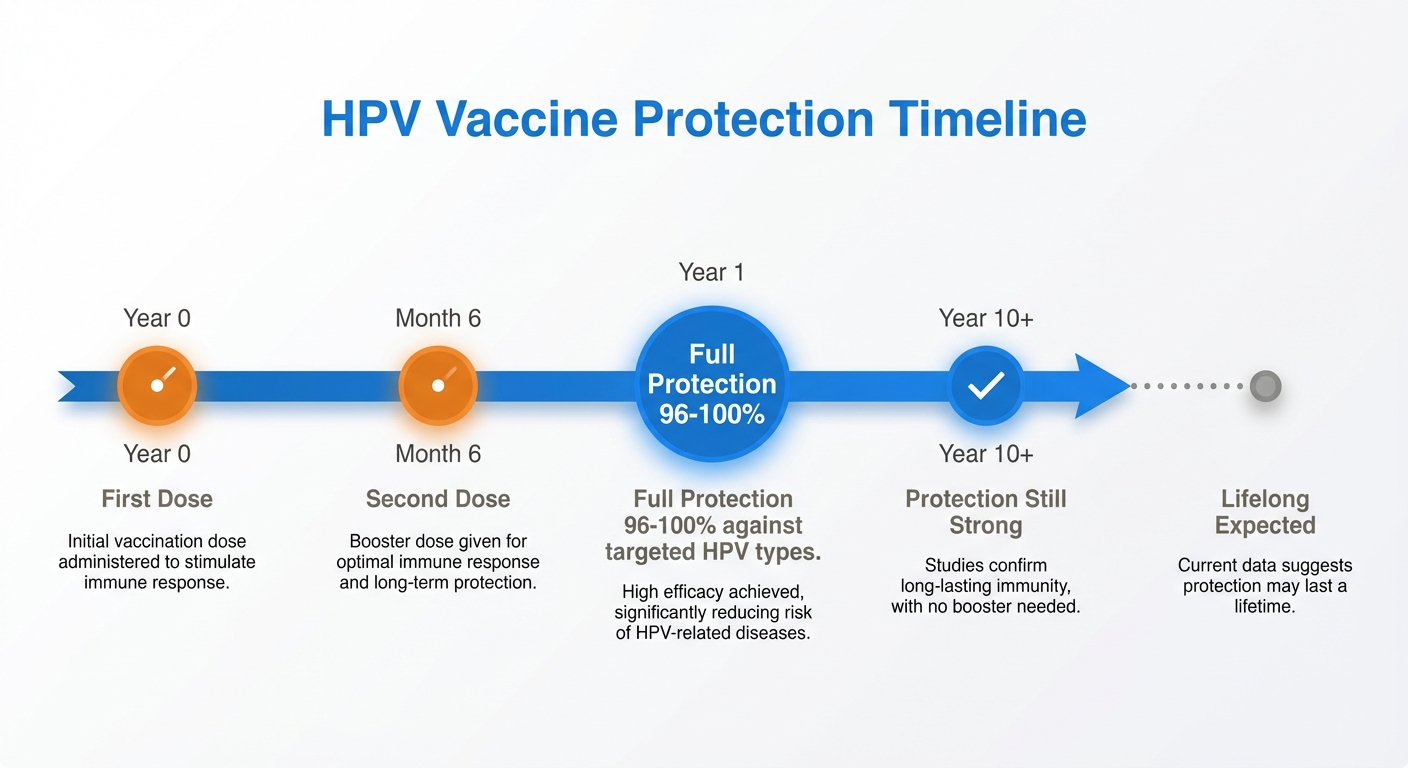
How Long Does Protection Last?
One concern about cervical cancer prevention is whether protection wanes over time. The evidence is reassuring.
Current Duration Data
Studies tracking vaccinated individuals show:
- 10+ years protection confirmed from clinical trial data
- Antibody levels remain high with no signs of waning
- No booster currently needed based on current evidence
- Lifelong protection expected based on antibody persistence patterns
The oldest vaccinated individuals have now been followed for 15+ years, and protection remains excellent.

Why Protection Appears Permanent
HPV vaccine generates:
- Very high initial antibody levels (10-100 times higher than natural infection)
- Long-lived memory B cells that can rapidly produce antibodies if needed
- Stable antibody persistence unlike some vaccines that show declining levels
Compare to natural HPV infection:
- Natural infection often fails to generate strong immunity
- People can be reinfected with the same HPV type
- Antibody levels after natural infection are low
The vaccine creates better, longer-lasting immunity than natural infection does.
Booster Doses
Currently, no booster dose is recommended because:
- Antibody levels remain high 10+ years post-vaccination
- No breakthrough cervical cancers in vaccinated populations
- No evidence of waning protection
If protection waned, we’d see:
- Rising HPV infection rates in vaccinated groups (we don’t)
- Increasing cervical pre-cancers in vaccinated women (we don’t)
- Declining antibody levels (we don’t)
Future evidence might change recommendations, but current data suggests protection is lifelong. At our London clinic, we follow the latest NHS and JCVI guidance on HPV vaccination schedules.
Do You Still Need Cervical Screening After HPV Vaccine?
Yes, absolutely. Here’s why.
Why Screening Remains Important
The HPV vaccine prevents 90% of cervical cancers, not 100%. You still need screening to catch:
Rare HPV types not covered by the vaccine (10% of cervical cancers)
Cancers from non-HPV causes (extremely rare but possible)
Pre-cancers that developed before vaccination (if vaccinated as adult)
Current UK Screening Guidelines
All women aged 25-64 in London and across the UK need cervical screening:
- Ages 25-49: Every 3 years
- Ages 50-64: Every 5 years
This applies regardless of vaccination status. Vaccinated women need screening at the same intervals as unvaccinated women.
What Changes for Vaccinated Women
In the future, screening guidelines may change for fully vaccinated cohorts:
- Longer intervals between screens possible
- Starting screening later (after age 30) under consideration
- HPV testing instead of cytology becoming standard
But for now, follow current screening guidelines.
Combining Prevention Methods
Think of cervical cancer prevention as layers of protection:
- HPV vaccination: Prevents 90% of cases
- Cervical screening: Catches the remaining 10% early
- Prompt treatment of abnormalities: Stops pre-cancer becoming cancer
Together, these make cervical cancer almost entirely preventable.
Common Concerns About Vaccine Effectiveness
“I’ve read the vaccine doesn’t work”
This confusion comes from misunderstanding clinical trial data. Early trials couldn’t show cervical cancer prevention directly because:
- Cancer takes 10-20 years to develop
- Can’t ethically wait that long for trial results
- Trials measured pre-cancer (CIN2/3) instead
Those trials showed 96-100% prevention of pre-cancers. Now, 15+ years later, real-world data confirms cervical cancer prevention.
“The vaccine only works for a few years”
This myth persists despite evidence showing:
- No decline in protection after 15 years
- Stable antibody levels
- Zero breakthrough cancers in vaccinated groups
The confusion may come from other vaccines (like flu) that need annual boosters. HPV vaccine doesn’t.
“You can still get cervical cancer after vaccination”
True, but the risk is reduced by 90%. For women vaccinated at 12-13, the risk appears to be zero based on current data. For older vaccinated women, the risk is dramatically lower than unvaccinated women.
Saying “you can still get cervical cancer” is like saying “you can still die in a car crash while wearing a seatbelt.” True, but the risk reduction is so massive that prevention is clearly worthwhile.
“The vaccine has serious side effects”
Serious side effects occur in less than 1 in 10,000 doses. Compare this to cervical cancer risk in unvaccinated women (1 in 135 in the UK). The vaccine is far safer than the disease it prevents.

The Bottom Line: Does HPV Vaccine Prevent Cervical Cancer?
Yes. The evidence is unequivocal:
- 90% of cervical cancers prevented by Gardasil 9
- Zero cervical cancers in women fully vaccinated at 12-13 (England study of 28,000+ cancers)
- 87% reduction in cervical pre-cancers in vaccinated populations
- Protection lasting 10+ years with no sign of waning
- Effectiveness even in adults aged 25-45
The HPV vaccine is one of the most effective cancer prevention tools in medicine. It’s the only vaccine that prevents cancer directly by stopping the infection that causes it.
Ready to Get Protected?
The evidence shows HPV vaccine prevents 90% of cervical cancers with zero cases in fully vaccinated women. At Ealing Travel Clinic in West London, we provide Gardasil 9 vaccination for £150 per dose. Most people need 2 doses (£300 total) given 6 months apart. Call 0208 567 0982 or visit us at 30 Northfield Avenue, London W13 9RL for same-day appointments.
Getting HPV Vaccine in London at Ealing Travel Clinic
Now you know the vaccine works. Ready to book your HPV vaccine in London?
Why Choose Us
Same-day appointments often available
£150 per dose with no hidden fees
Convenient West London location serving Ealing, Acton, Hanwell
Saturday appointments for those working weekdays
Located in West London, we’re easily accessible from Ealing Broadway, Acton, Hanwell, and surrounding areas. Our clinic serves London residents who want evidence-based HPV vaccination with transparent pricing and expert care.
What You Need to Know
Dosing: Most people need 2 doses, 6 months apart
Cost: £150 per dose (£300 total)
Time: Brief consultation, vaccination, 15-minute observation
Booking: Call 0208 567 0982 or book online
The evidence is clear. The vaccine prevents cervical cancer. The only question is when you’ll get protected.
Learn more about HPV vaccination including full pricing, scheduling, and what to expect at your appointment.
Frequently Asked Questions
Book Your HPV Vaccine in London
Ready to get protected against cervical cancer?
Now you know the evidence: the HPV vaccine prevents 90% of cervical cancers, with zero cases in women vaccinated at the recommended age. The research is clear, the protection is proven, and the decision is straightforward.
Book your HPV vaccination at Ealing Travel Clinic. £150 per dose, most people need 2 doses (£300 total). No hidden fees, no surprise charges, just transparent pricing for cervical cancer prevention.
Take the next step: Read our comprehensive HPV vaccine London guide for complete information about booking your vaccination at Ealing Travel Clinic.
Book with confidence:
- Phone: 0208 567 0982
- Visit: Ealing Travel Clinic, 30 Northfield Avenue, London W13 9RL
- Book Online: Click Here to Book Your HPV Vaccine
Stop researching. Start protecting. Same-day appointments available for West London residents.
Table of Contents
- The Evidence: How Well Does HPV Vaccine Prevent Cervical Cancer?
- How Does HPV Vaccine Prevent Cervical Cancer?
- Does HPV Vaccine Work If You’re Already Sexually Active?
- How Long Does Protection Last?
- Do You Still Need Cervical Screening After HPV Vaccine?
- Common Concerns About Vaccine Effectiveness
- The Bottom Line: Does HPV Vaccine Prevent Cervical Cancer?
- Getting HPV Vaccine in London at Ealing Travel Clinic
- Frequently Asked Questions
- Book Your HPV Vaccine in London